Simplify Your Billing
Artemis helps billing teams stay ahead of denials, delays, and manual work. With smart automation and real-time visibility, you can focus on clean claims, faster payments, and better collaboration.





4.7 / 5.0

Customer Reviews
Eligibility Checks Made Easy
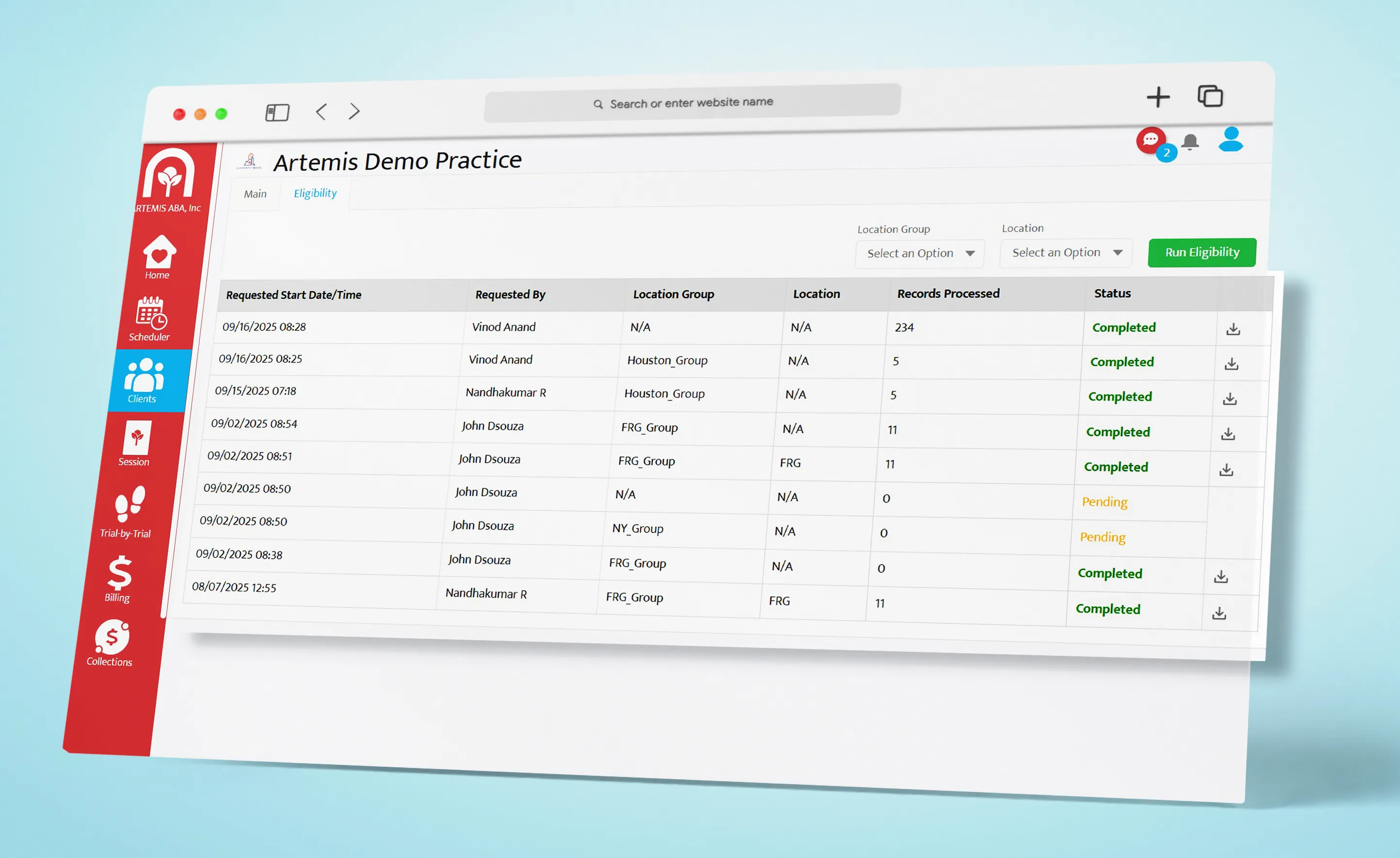
Verify a client’s benefits before billing to avoid coverage-related denials. Artemis automates eligibility checks, whether you're checking one client or running bulk verifications. so claims are clean from the start and coverage details are never a bottleneck.
Real-Time Authorization Tracking
Stay within payor-approved limits with real-time tracking of authorization units. This ensures your team doesn’t exceed what’s approved, helping you avoid costly denials and maintain compliance effortlessly.
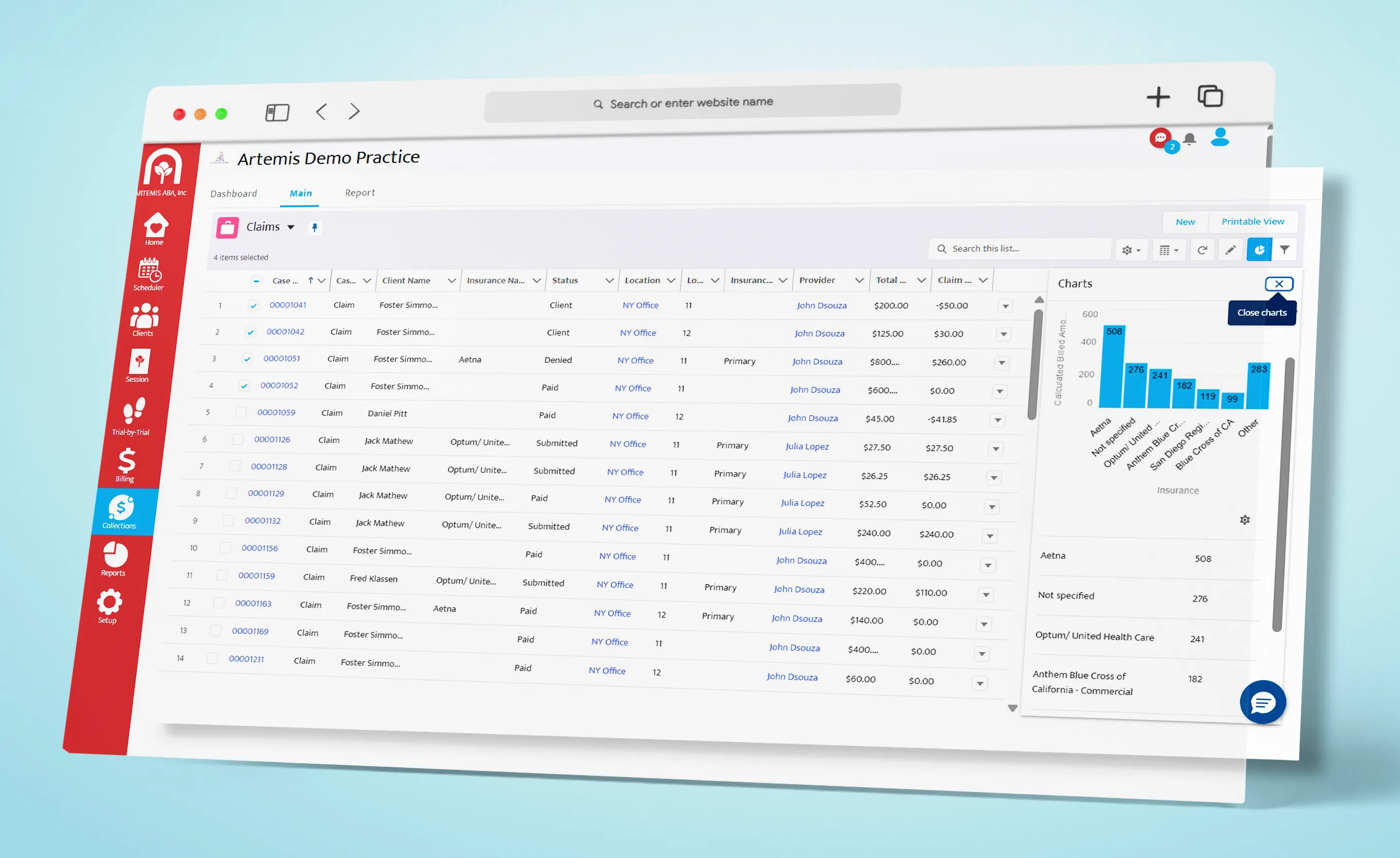
Intelligent Claims Dashboard
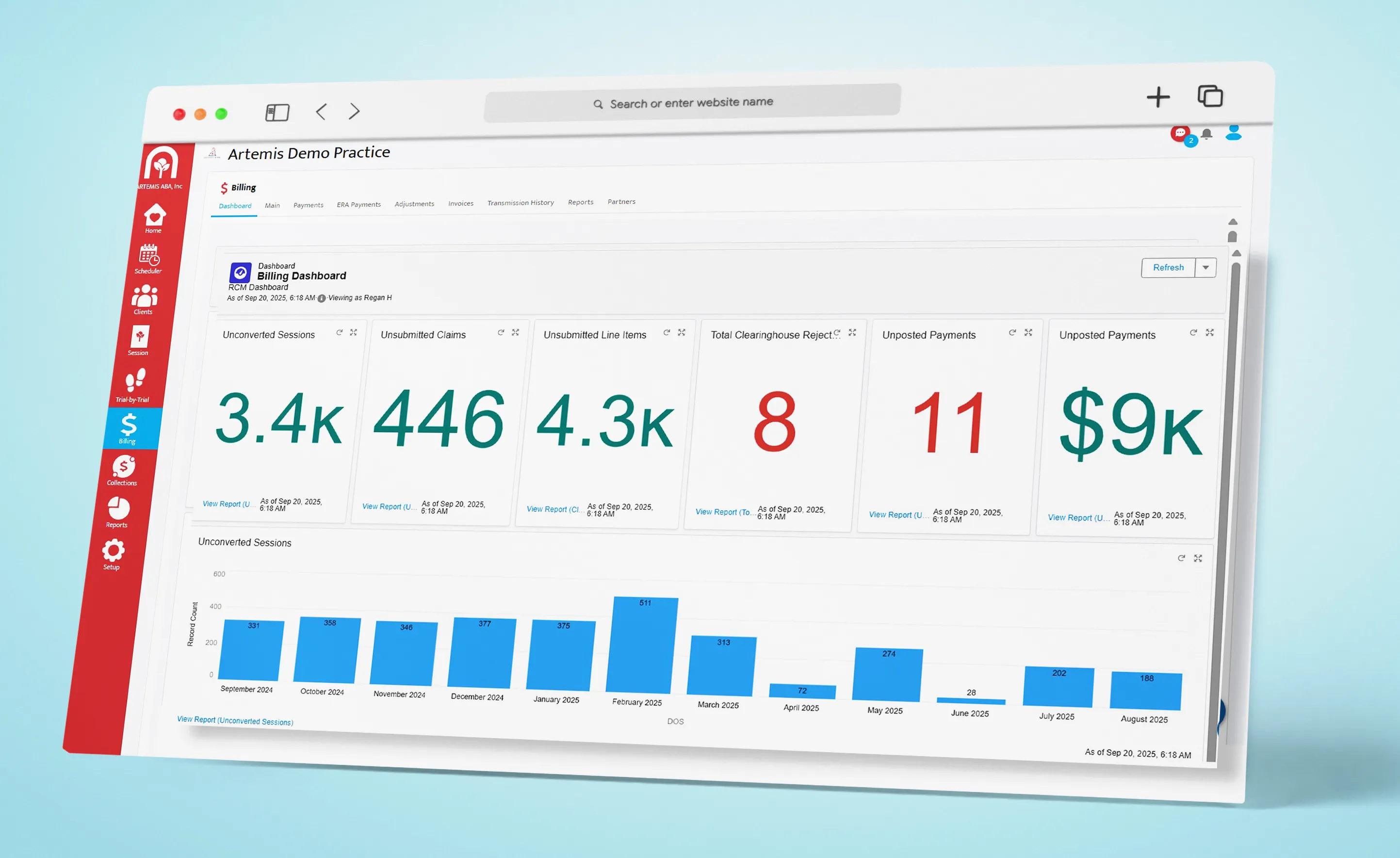
Get full visibility into every claim, pending, submitted, or paid, so you can prioritize your work efficiently. The dashboard makes it easy to track progress and stay focused on what needs attention.
Advanced Claim Search
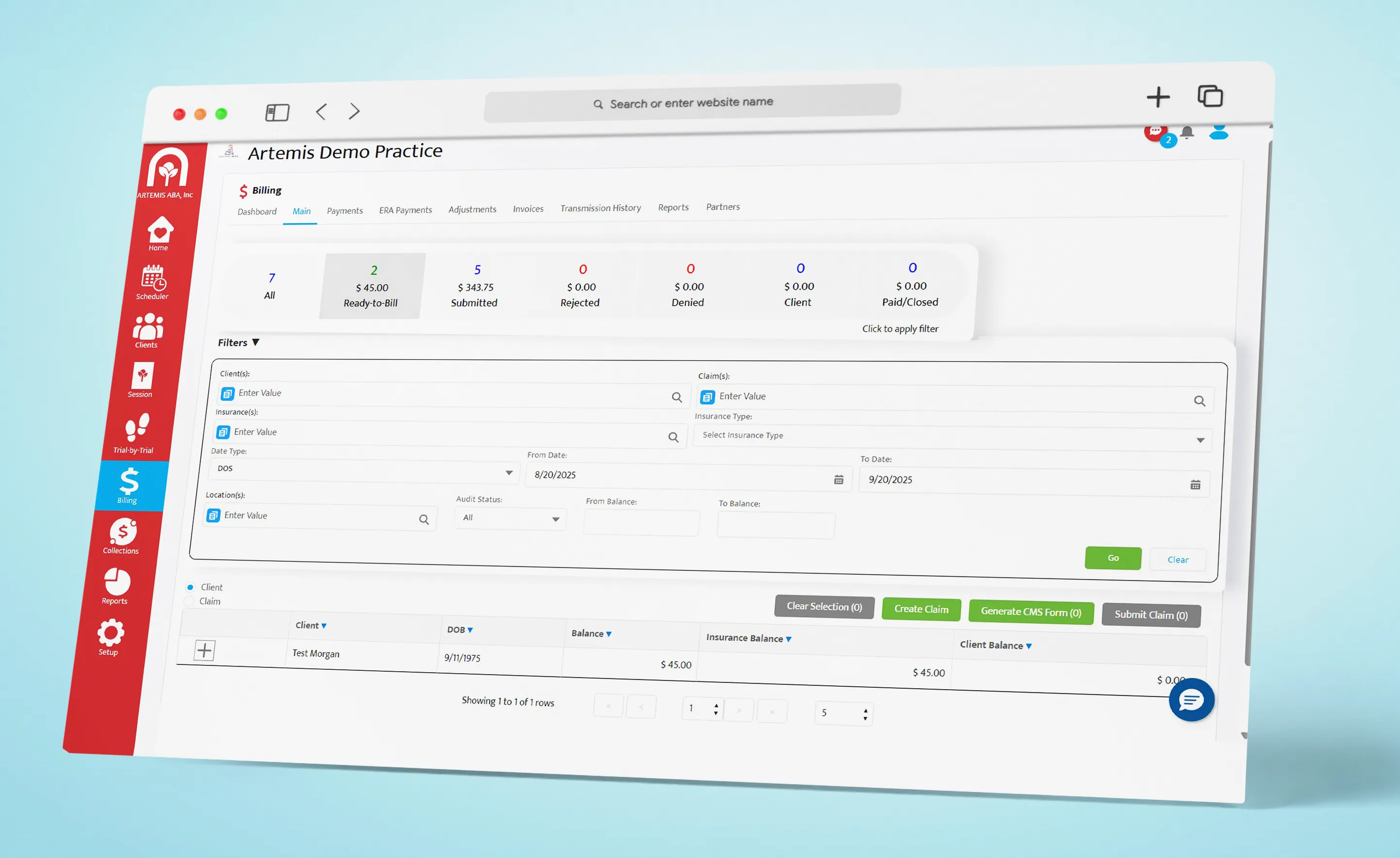
Quickly search for claims by CPT code, modifier, or client to troubleshoot payor issues faster. These advanced filters reduce guesswork and help you resolve problems with precision.
ERA Payment Posting
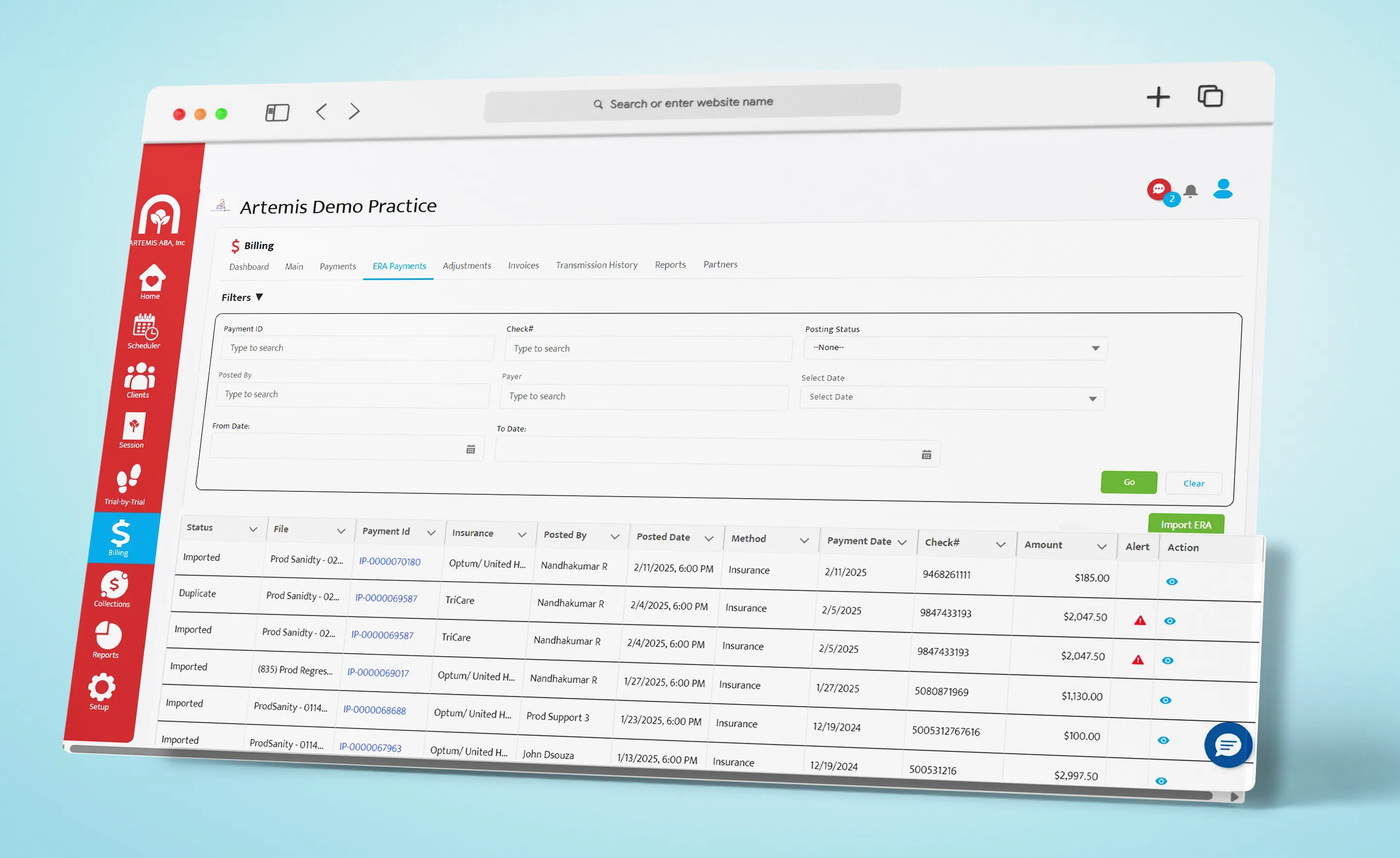
Post payments instantly from ERA files to keep balances and reports accurate. Artemis eliminates manual entry, speeding up reconciliation and ensuring your financial data stays clean.
Deposit Matching & Reconciliation
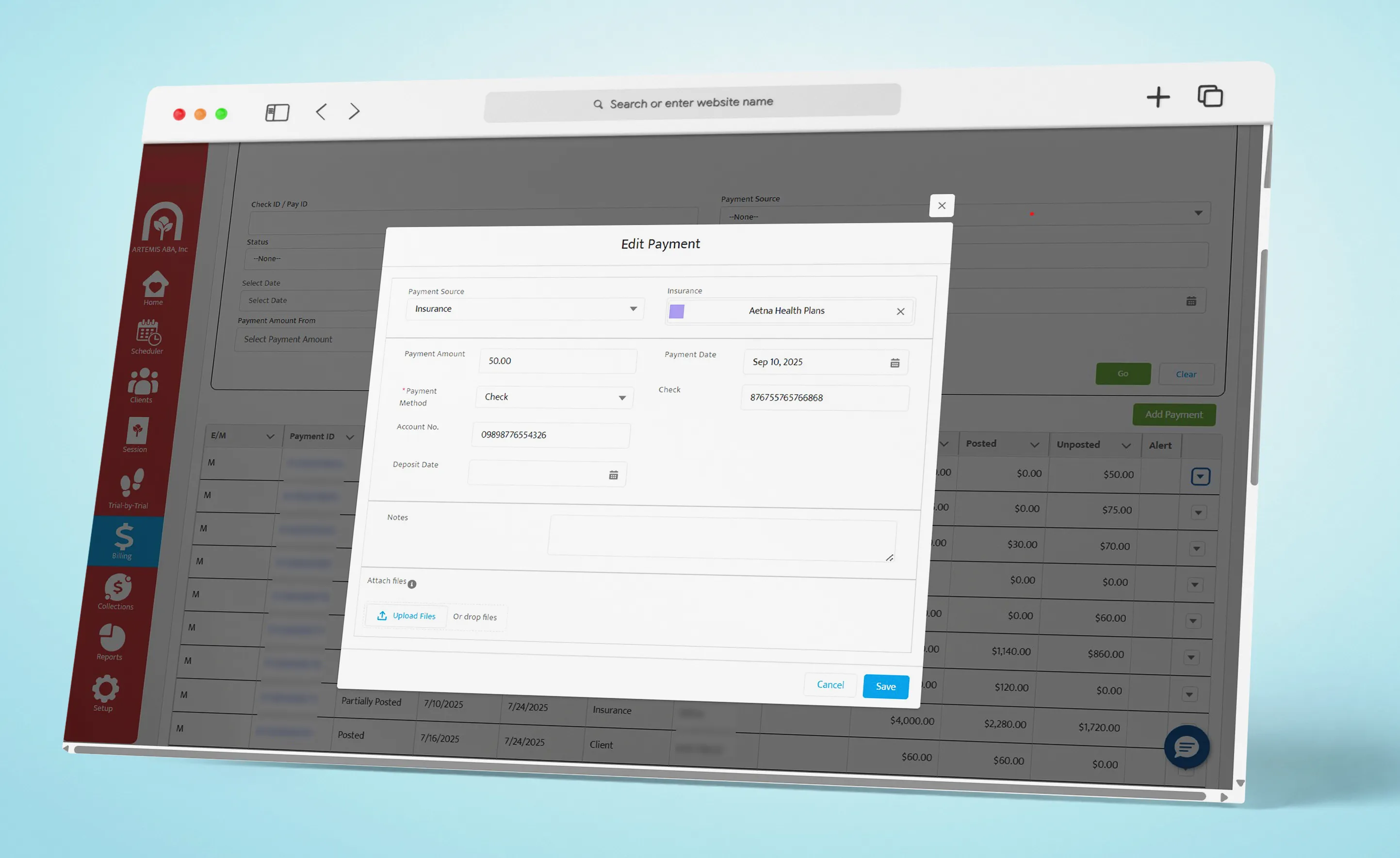
Automatically match deposits with posted payments using tracked deposit and payment dates. This saves time and removes the need for manual reconciliation, keeping your records aligned.
Denial Management & Escalation
Denials are flagged the moment they occur, with payor-specific reason codes explained in plain language, no more guessing what “CO-45” means. You can assign these denials to team members, track progress with notes, and escalate issues to the RCM or appeals team without delay.
Denial Assignment & Tracking
Assign specific denials to team members and track their progress with ease. Each denial can be monitored with notes and status updates, keeping everyone aligned and ensuring timely resolution without delays.
Payor-Specific Denial Trends
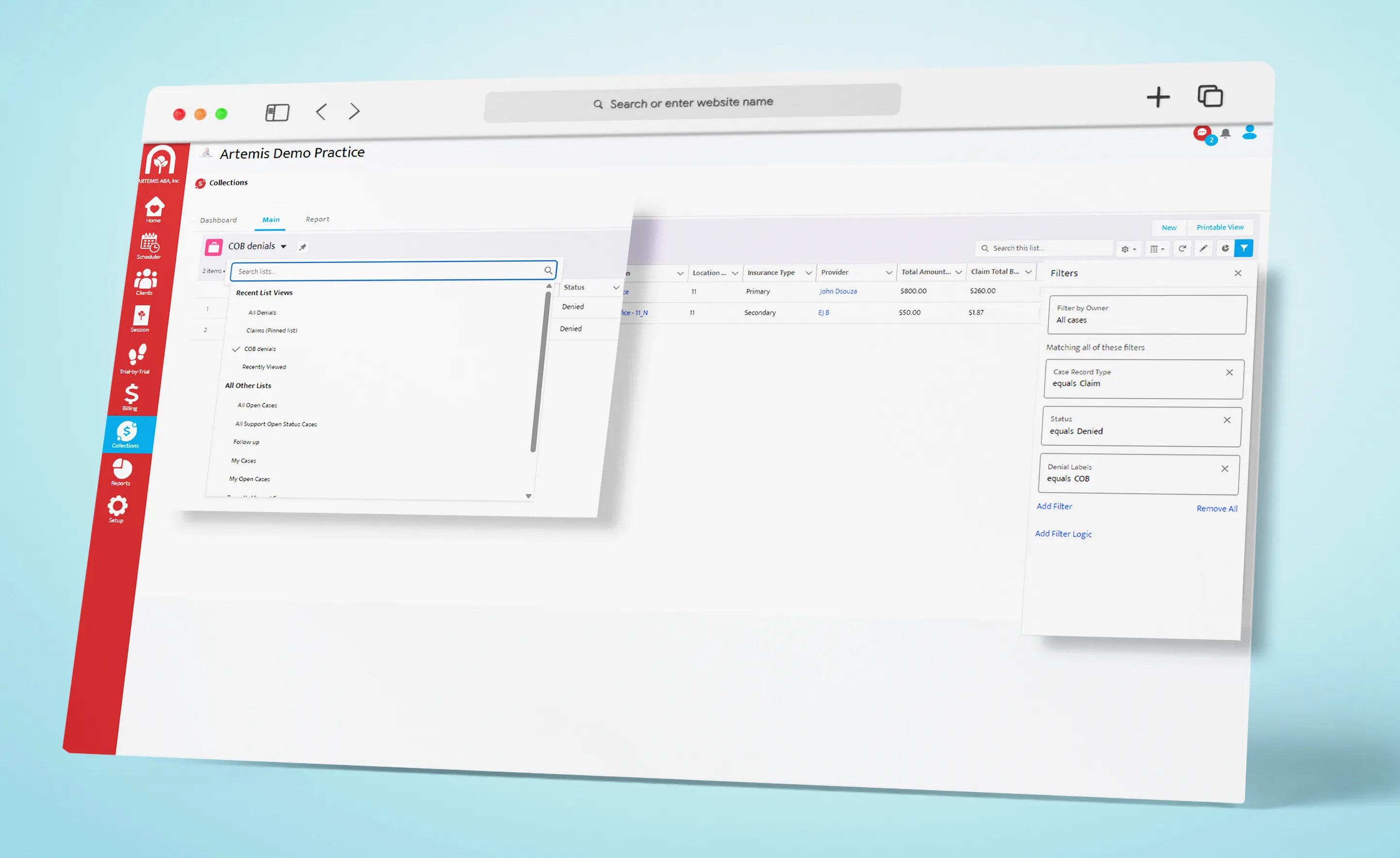
View denial trends by payor to proactively reduce future rejections. These insights help you optimize collections and strengthen your revenue cycle strategy.
Aging & AR Reports
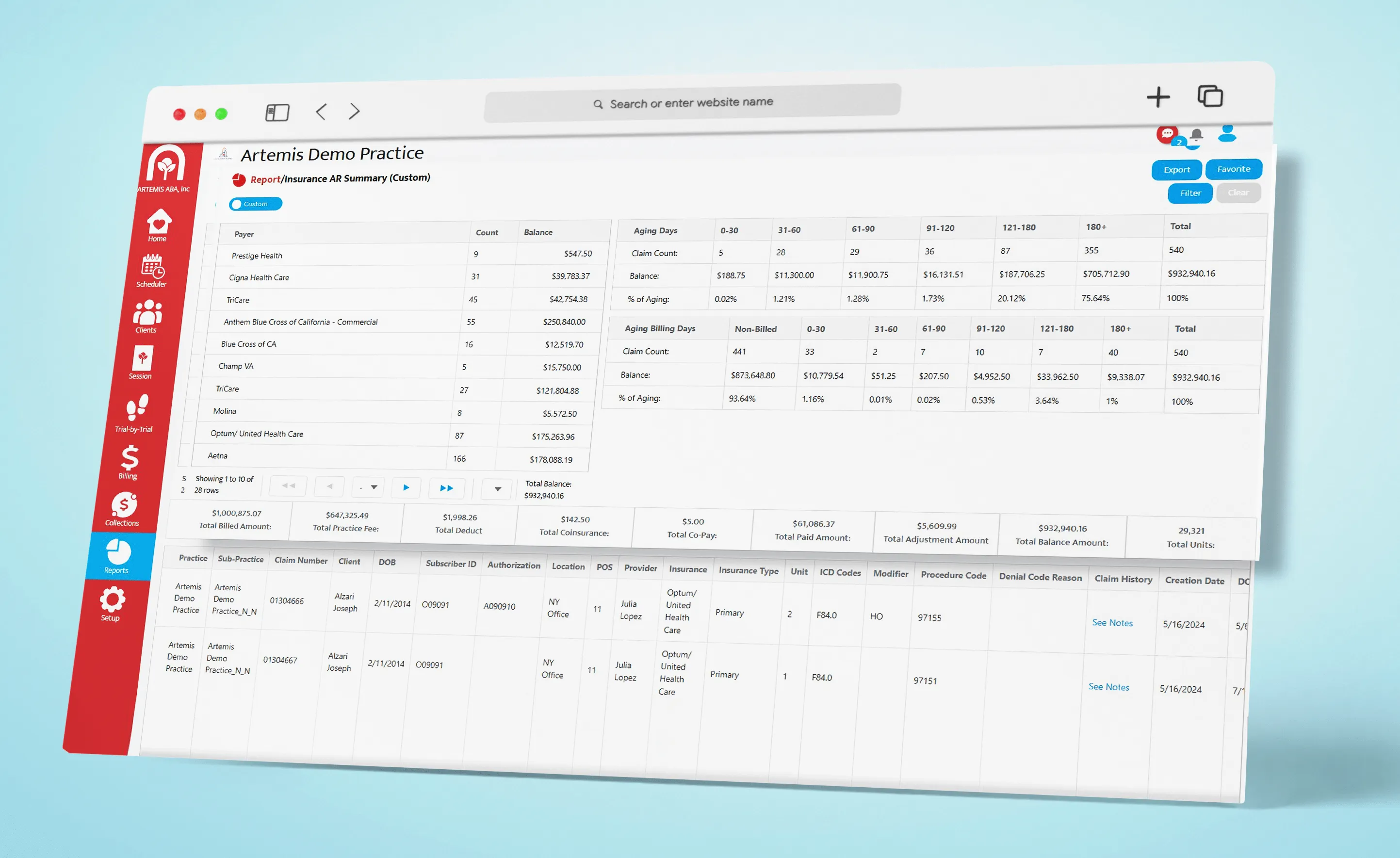
Generate aging and AR reports quickly to show leadership where cash flow is delayed. Artemis provides actionable financial data that supports smarter decision-making and transparency.
Clinical & Billing Unified Dashboard

Share a unified dashboard with the clinical team to ensure claims are sent out on time. This real-time collaboration keeps therapy delivery and billing requirements in sync.
Session Note Validation
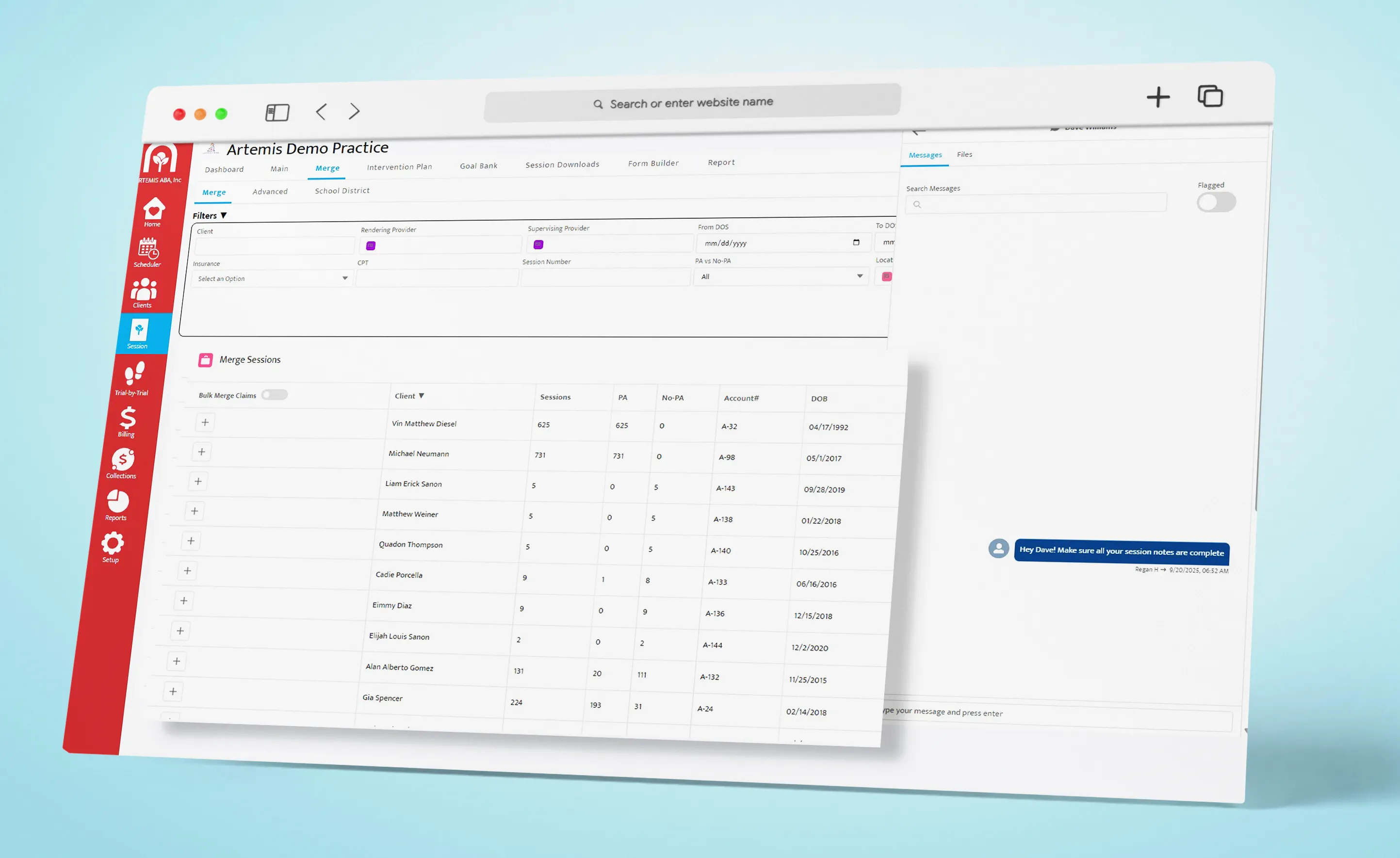
Flag missing or incorrect session notes instantly so clinicians can correct them before submission. This prevents billing errors and keeps claims moving without delays.
With Artemis ABA, billers can work smarter, not harder, with tools that eliminate guesswork and reduce delays. From eligibility to collections, every step is streamlined so your team can stay focused, accurate, and ahead of the curve.






%201.webp)


